Download PDF:
Whole Body + Local Cryotherapy Reduces Muscle Spasticity
Efficacy of cold therapy on spasticity and hand function in children with cerebral palsy
Gehan M. Abd El-Maksoud, Moussa A. Sharaf, Soheir S. Rezk-Allah Show
Abstract
Spasticity remains a major cause of disability among children with cerebral palsy (CP). Effective management depends on careful assessment and an interdisciplinary treatment approach. The purpose of this study was to investigate the effect of cold therapy when used in combination with conventional physical and occupational therapy to control upper limbs’ spasticity and to improve hand function in children with spastic CP. Thirty children of both sexes (12 girls and 18 boys) with spastic CP with ages ranged from 4 to 6 years (mean age 62.2 ± 7.5 months) participated in this study. They had mild to moderate spasticity in elbow and wrist flexors. Children were randomly divided into two groups of equal number: group I and group II. Children in group I received cold therapy on elbow and wrist flexors immediately before the application of conventional physical and occupational therapy. Those in group II received the same conventional occupational and physical therapy only. In both groups treatment was conducted three times per week for a successive 3 months. Spasticity, range of motion (ROM) and hand function were evaluated before and after the treatment by using the Modified Ashworth Scale, the electronic goniometer and the Peabody Developmental Motor Scale, respectively. Both groups showed a statistically significant reduction in spasticity, increase in ROM and improvement of hand function but group I showed a more significant improvement. It can be concluded that cold therapy in conjunction with conventional physical and occupational therapy significantly reduced spasticity, increased ROM and improved hand function in children with spastic CP.
Introduction
Spasticity is a widespread problem in cerebral palsy (CP) as it affects function and can lead to musculoskeletal complications [1]. It occurs as a result of pathologically increased muscle tone and hyperactive reflexes mediated by a loss of upper motor neuron inhibitory control [2].
Children with CP demonstrate poor hand function due to spasticity in the wrist and finger flexors [3]. Thus spasticity in the flexor muscles of the upper limbs poses a great deal of functional limitation in the hands. One common problem associated with poor hand function as a result of spasticity is the inability of the child to grasp objects and difficulty with fine motor tasks such as writing or cutting with hands [2], [3].
The management of upper limbs’ problems in CP is often complex and challenging. Effective treatment requires a multidisciplinary approach involving paediatricians, occupational therapists, physiotherapists, orthotists and upper extremity surgeons. Interventions are generally aimed at improving function and cosmoses by spasticity management, preventing contractures and correcting established deformities. Treatment objectives vary according to each child and range from static correction of deformities to ease nursing care, to improvement in dynamic muscle balance to augment hand function [4].
Previous studies have reported various treatment approaches and modalities to manage spasticity associated with spastic CP and other upper motor neuron lesion disorders. These include the use of oral neuropharmacological agents, injectable materials such as botulinum – a toxin or surgical treatment. The other treatment approaches are contracture reduction, orthosis, topical anesthesia application using various massage techniques, strengthening the antagonist musculature with electrical stimulation and the application of cryotherapy or ice therapy [5], [6].
Ice or cold therapy is a widely used treatment technique in the management of acute and chronic conditions of various types. There are many tissue-based effects which are promoted by the application of cold therapy and these include post-injury reduction of swelling and oedema, an increase in the local circulation, lowering of the acute inflammation that follows tissue damage, muscle spasm reduction, and pain inhibition. Muscle contraction can be facilitated by using cold therapy and this can be used to improve muscle contraction to increase joint ranges of motion after injury. Another effect of cold is a time-related reduction in spasticity once the cold has been applied for some time. Cold can be applied to the body in three different ways: immersing in cold water, rubbing with ice cubes or ice packs or using evaporative sprays such as ethyl chloride [7].
The ability of muscles to function after spasticity reduction varies. Treating spasticity does not always facilitate the acquisition of undeveloped skills. The importance of physical and occupational therapy intervention for achieving functional goals cannot be overemphasized [8].
This study was therefore designed to investigate the effect of cold therapy when used in combination with conventional physical and occupational therapy to reduce upper limbs’ spasticity and improve hand function in children with spastic CP.
Subjects and methods
Subjects
Thirty children with spastic CP (18 diplegia and 12 quadriplegia), with ages ranged from 4 to 6 years (mean age 62. 2 ± 7.5 months), participated in this study after their parents signed consent forms for their children’s participation. They were selected from the outpatient clinic of the Faculty of Physical Therapy, Cairo University.
Children were enrolled in this study if they met the following criteria: a mild to moderate degree of spasticity in the elbow and wrist flexors; ranged from grade 1+ to grade 3 according to the Modified Ashworth Scale (MAS) [9]; ability to sit alone or even with support; sufficient cognition to allow them to follow simple verbal commands and instructions during tests and training; and normal skin sensation of the upper limbs.
Children were excluded from the study if they had fixed contractures or deformities in the upper limb, concurrent therapy with oral antispastic drugs, previous treatment with botulinum toxin injection, alcohol or phenol into upper limbs, previous surgical intervention in the upper limbs, vasospasm or cold urticaria, visual or auditory defects or autistic features. The study was approved by the ethical committee of the Faculty of Physical Therapy, Cairo University.
The participants were randomly divided into two groups (group I and group II) of equal numbers. Group I consisted of 15 children with spastic CP (five girls and ten boys), nine with diplegia and six with quadriplegia. Their mean age was 63.2 ± 7.4 months. They received cold application on the area of upper arm and flexor compartment of the forearm (elbow and wrist flexor muscles) immediately before the application of the conventional physical and occupational therapy programme. Group II consisted of 15 children with spastic CP (seven girls and eight boys), nine with diplegia and six with quadriplegia. Their mean age was 61.2 ± 7.7 months. They received the same physical and occupational therapy programme only.
Procedures
Evaluative procedure
Each child was evaluated for degree of spasticity, ROM and fine motor skills. Spasticity was assessed by using MAS to quantify the degree of spasticity in the elbow and wrist flexors for all children in both groups. The degree of spasticity ranged from grade 1+ to grade 3 according to MAS. To accommodate the “1+” modification for numeric analysis, grade “1+” was recorded as 1.5 [10]. ROM of elbow and wrist extension was measured by the electronic goniometer. The Peabody Developmental Motor Scale (PDMS-2) was used to evaluate fine motor skills including grasping and visual motor integration. This scale provides a comprehensive sequence of gross and fine motor skills by which the therapist can determine the relative developmental skill level of a child, identify the skills that are not completely developed and plan an instructional programme that can develop those skills [11]. Assessment of these parameters was carried out before the commencement of training (pre-treatment) and at the end of 3 months of treatment (post-treatment) for all children by the same examiner who was blinded regarding the group to which each child was assigned.
Treatment procedure
Group I
The children in this group were placed in a sitting position. The upper arm and entire forearm were carefully and decently exposed and skin sensation was assessed for all children to ensure that none of them had defective skin sensation. Two test tubes were used for this assessment, one filled with hot water and the other with cold water. The test tubes were randomly placed in contact with the skin area to be tested. The child was asked to indicate when a stimulus was felt and to report “hot”, “cold”, or “unable to tell” [12]. The area was then cleaned with cotton wool and methylated spirit. The upper limb of the child was positioned on a pillow with the shoulder maintained in mild abduction by a tumble form. The forearm was also positioned in mid flexion and supination. Cold pack (Compress-Reusable cold gel back) was applied over a wet towel to the skin of the treated area to avoid excessive local cooling (ice burn); this pack was held in place by dry towelling. The skin under the cold pack was checked for a minute after applying it to look for abnormal reactions or unusual changes in skin colour. This was repeated after 5 min if no abnormal reactions were obvious in the initial inspection [13]. The cold pack was applied for 20 min, then removed and the skin dried [14], [15]. Immediately after cold application all children received the following physical and occupational programme for 2 h [16], [17], [18]. The cold therapy followed by the physical and occupational programme was applied three times per week for a successive 3 months.
Physical and occupational therapy programme
All children participating in this study received the same physical and occupational therapy programme lasting for 2 h/session, three sessions per week over a successive 3 months. This programme included manual passive stretching for elbow and wrist flexors, which was based on the passive range of motion (PROM) therapeutic exercises described by Kisner and Colby [19]. The PROM consisted of moving the elbow, wrist, fingers and thumb passively into extension and holding this position for 60 s. This procedure was repeated five times giving a total duration of 5 min. Hand weight bearing (HWB) exercises for both upper limbs, as ROM exercises and as proprioceptive training, were also applied from positions of sitting or side sitting on a mat and/or sitting on a roll. Additionally, protective extensor thrust (PET) was provided from sitting on a roll and prone on a ball to stimulate the extensor pattern of the upper limbs. Furthermore, strengthening exercises for the antispastic muscles (elbow and wrist extensors) using different toys and motivation to encourage the child to perform the desired exercises, were also part of our programme.
Exercises facilitating hand skill patterns included basic reach, grasp, carry and release and the more complex skills of in-hand manipulation and bilateral hand use. The child sat on a chair-table and the therapist sat at the side to guide and assist the child to perform the exercises correctly. The exercises included the following:
- Reach with both hands and then by each hand for an object presented at midline.
- Reach with 45° and 90° of shoulder flexion, neutral rotation of humerus, elbow extension and forearm supination to mid position.
- Reach across midline while keeping an erect trunk.
- Use a sustained palmer and pincer grasp with wrist extension.
- Release objects into container at arm length from the child’s body to encourage elbow and wrist extension.
- Use both hands together to push, carry or lift large object to encourage elbow and wrist extension.
- Throw ball unilaterally or bilaterally to encourage the extensor pattern of upper limbs.
Group II
Children in this group received only the same physical and occupational therapy programme given to group I without the prior cold therapy.
Data analysis
Descriptive statistics of mean and standard deviation presented the children’s ages, MAS scores, ROM and fine motor quotient (FMQ). Non-parametric tests (the Wilcoxon signed-rank test and the Mann–Whitney test) were used to analyze the pre- and post-treatment values of MAS and FMQ within and between the groups. The paired and unpaired t-test was used to compare the pre- and post-treatment values of ROM of elbow extension and wrist extension within and between the groups. A P-value of less than 0.05 was taken as significant.
Results
Thirty children with spastic CP (18 with diplegia and 12 with quadriplegia) were enrolled in this study. Twelve (40%) of them were girls and 18 (60%) were boys. Their ages ranged from 4 to 6 years. Both upper limbs were treated, but only the dominant arm was included for analysis.
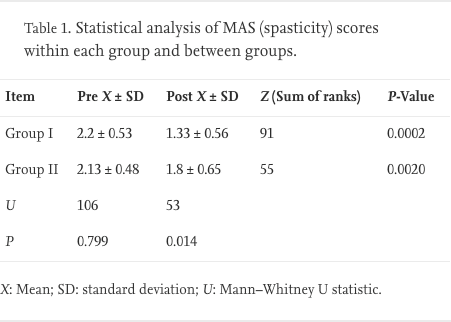
Spasticity
Comparison of the pre- and post-treatment MAS scores for group I revealed a significant reduction in spasticity (P = 0.0002) in 13 children while in the remaining two subjects the scores remained constant. Comparison of the pre- and post-treatment MAS score for group II showed a significant reduction in spasticity (P = 0.002) in 10 of the children while in the remaining five the scores remain unchanged. The analysis between the groups, using the Mann–Whitney test, showed no significant difference in the spasticity scores pre-treatment (P = 0.7992), while there was a significant difference in the spasticity scores post-treatment in favour of group I (P = 0.0143) (Table 1).
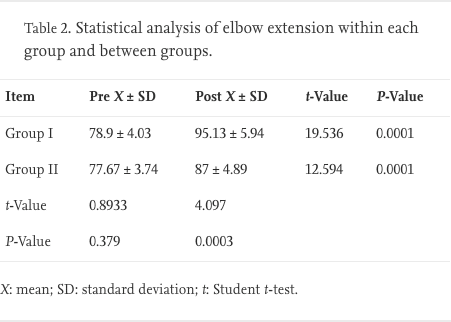
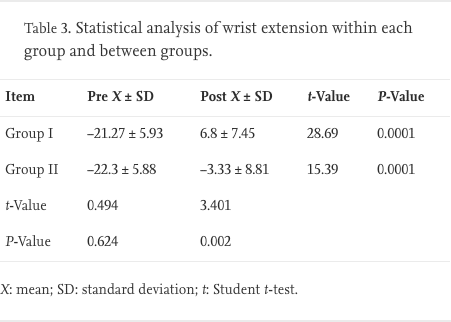
Range of motion
Range of motion was assessed using the electronic goniometer according to the Norkin and White procedure [20]. Three repetitions were performed at both the elbow and the wrist. We concentrated on joint extension as extension is commonly more problematic in spasticity than is flexion.
Comparisons of the pre- and post-treatment values of ROM of elbow and wrist extension were made using the paired t-test. The results showed a significant improvement in both groups in elbow extension and wrist extension (P < 0.0001). The analysis between the groups using the unpaired t-test showed no significant difference in ROM of elbow and wrist extension pre-treatment (P = 0.3793 and 0.6247, respectively), while there was a significant difference in post-treatment values of ROM of elbow and wrist extension between the groups in favour of group I (P = 0.0003 and 0.0020, respectively) (Table 2, Table 3).
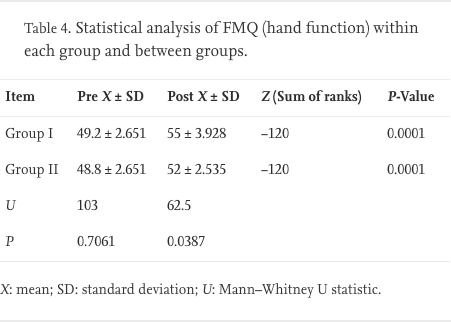
Hand function
The Peabody Development Motor Scale was used to evaluate the hand function for children in this study. Fine Motor Quotient (FMQ), which is the most reliable score yielded by this scale, was used to measure the changes in-hand function (grasping and visual motor integration) after our intervention.
Comparison of the pre- and post-treatment values of FMQ, using the Wilcoxon test, revealed a significant improvement in both groups (P < 0.0001). The analysis of FMQ values pre- and post-treatment between the groups, using the Mann–Whitney test, revealed no significant difference in pre-treatment results (P = 0.7061), while there was a significant difference in the post-treatment results in favour of group I (P = 0.0387) (Table 4).
Discussion
The results of this study showed a significant improvement in both groups in all measuring variables (MAS for spasticity, ROM of elbow and wrist extension, FMQ for hand function) after 3 months of treatment. However, higher improvement was achieved in group I in all measuring parameters. In agreement with many reports [14], [21], [22], [23], [24], [25], [26], the results of this study indicate that cold therapy is an acceptable method for the temporary relief of spasticity. In addition the present study proved that cold therapy is effective when combined with physical and occupational therapy in reducing spasticity and improving hand function in children with spastic CP.
In this study, it was intended to apply the cold therapy for 20 min on elbow and wrist flexors, aiming to gain significant and long duration reduction in spasticity, as an adequate period of time was needed for subsequent ROM exercises and training of fine motor skills without interference of spasticity. In most of the children (n = 13), the spasticity reduced for 60–90 min after cold application. This is supported by the findings of Miglietta [24] who studied the effect of cooling on clonus in 40 spastic patients. He found that clonus had reappeared in 100% of patients 90 min after cold treatment stopped.
The results of this study showed a significant reduction in spasticity in both groups, which may be due to stretching of elbow and wrist flexor muscles through manual passive stretching and hand weight bearing. Both provided continuous stretching of those muscles, which led to fatigability of stretch receptors and decreased its response to any stimulus; this also led to breakdown of the contracture, which allowed more lengthening of muscle fibres, which counteracts the effect of spasticity. Moreover, approximation of the upper limb via hand weight bearing inversed the proprioceptive reflex in the upper limb and added more inhibition to the spasticity in the elbow and wrist flexors.
The post-treatment results of MAS revealed a significant difference between the groups in favour of group I. This difference may be attributed to the effect of cold therapy on reducing spasticity. There are many possible underlying mechanisms that explain how cold therapy reduces spasticity. The first mechanism was explained by Eldred et al. [27], Ottosn [25], and Knutsson and Mattsson [26] who reported that ice application reduces muscle tone through a reduction of spindle sensitivity. They found that the rate of spontaneous spindle discharge decreases with decreasing temperature. Also, the rate of discharge from the Golgi tendon organs was found to be temperature-dependent. The change in discharge of the muscle spindle may result from the effect of cold on extrafused muscle, the intrafusal fibres or the sensory endings. Similarly, Michlovitz et al. [28] stated that inhibition occurring due to the use of cryotherapy may be due to the local cooling effect on every component of the segmental sensorimotor complex, including large afferent fibres of muscle spindles (both alpha and gamma motoneurons), all skin receptors, extrafusal muscle fibres and the myoneural junction. The second possible mechanism is explained by Lippold et al. [29] who suggested that the effect of cold application is related to the role of change in membrane polarization. They found that hyperpolarization or low potassium concentration reduced or abolished spindle discharge. Also, their findings are in agreement with those of Eldred et al. [27]and associates who concluded that the site of thermal effect is the sensory terminal itself and is likely to be the result of change in membrane stability similar to those included in axons by lowering the temperature. Finally, Miglietta [24] reported that clonus and spasticity are not abolished unless the muscle temperature drops significantly. He mentioned the possibility that sympathetic fibres stimulation by cold application not only produces vasoconstriction but also decreases spindle sensitivity.
The results of this study revealed that most of the children (13) treated with cold therapy had a significant reduction in spasticity, while the remaining two children’s MAS scores remained constant. It may be argued that these children had little spasticity (grade 1+ on MAS) to remedy by cold therapy or that the deep muscle cooling was not achieved and insufficient cooling occurred. This agrees with Urbscheit et al. [30] who investigated the changes in H-response and the Achilles tendon jerk in hemiplegic patients after cold application. They found that the hemiplegic patients responded differently. The author suggested that local cooling might decrease, increase, or exert no effect on the spasticity.
The results of this study support the findings of Warren et al. [31] who concluded that deep prolonged and penetrating cold could be used in therapy to induce relaxation. They attributed their findings to be due to lowering of the background level of stretch afferent input. They reported that deep cold (penetrating the muscle mass) produces cold block of the receptors or the afferent fibres themselves.
The previous work of Price et al. [21] on the effect of cryotherapy on spasticity at the human ankle supports our results. They established that cryotherapy has an effect on reducing the path length, a parameter indicating the frequency dependent viscoelastic response at the ankle. High values of path length have been shown to be associated with the presence of spasticity. They recommended the use of cryotherapy for 1 h on the calf muscles aiming for spasticity reduction.
The results of this study confirm the findings of Lehman and de Lateur [14] who reported that cold application has been found useful to be used to reduce spasticity in upper motor neuron lesion and in muscle re-education to facilitate muscle contraction.
Regarding the ROM of elbow and wrist extension, there was a significant improvement in both groups. Increases of the extension of elbow and wrist joints may be due to reduction of flexors’ spasticity and strengthening of antagonistic muscles. Reduction of spasticity in elbow and wrist flexors provided less resistance to lengthening those muscles during the movement in the opposite direction, thus allowing more ROM. This explanation is supported by Exner [32] who reported that tightness of soft tissue found in spastic children could restrict movement and reduce the child’s ability to exhibit a normal ROM.
In addition, increases of the extension of elbow and wrist may be attributable to protective extensor thrust that facilitated the whole extensor pattern of upper limb including elbow and wrist extension. Moreover, hand weight bearing may also have a role in improving elbow and wrist extension. This agrees with Barnes [33] who found improvement of wrist extension in children with CP after upper limb weight bearing.
Higher improvement of ROM of elbow and wrist extensions in group I may be attributable to the effect of cold therapy. Cold therapy reduced spasticity of elbow and wrist flexors, which allowed the antagonistic muscles to work in an opposite direction without restriction from spastic agonist. Moreover, cold therapy reduced pain which encouraged the child to achieve maximum ROM as much as possible during strengthening exercises.
The results of this study agree with Knutsson [34] who found that passive resistance to stretching the chilled muscle was reduced and clonus was abolished. Also, he found that the strength of chilled muscles did not increase, but that the power of the antagonist was enhanced. The antagonist could function better because it was unopposed by the spastic muscles. Similarly, Lin [35] found that cold can facilitate increasing the range of motion in a joint. Also, Lehmann et al. [36] reported that in the management of spasticity, cold application can decrease tendon reflex excitability and clonus, increase ROM of the joints and improve the power of the antagonistic muscle group.
Concerning hand function, there was a significant improvement of FMQ in both groups. Improvement of hand function in both groups may be due to the combined effect of the physical and occupational therapy programmes. Reduction of flexor spasticity and increase of ROM of elbow and wrist extension, allowed the children to grasp and manipulate object in a more skillful manner. This is confirmed by the opinions of Brown et al. [37] and Francis et al. [38] who reported that reducing arm spasticity is associated with significant improvement in arm function.
Moreover, repetition of our occupational therapy programme over a successive 3 months helped the children in this study to improve their selective motor control and fine motor skills. During this period, the children started to construct sensory and motor memory about these skills that enabled them to become more skillful. This explanation agrees with Mclaughlin [39]who stated that repetitive activities guided by a therapist improve activities of daily living. This improvement may be due to the lying down of new engrams through repetitive activities.
Post-treatment results of FMQ (hand function) revealed a significant difference between the groups in favour of group I. This higher improvement may be attributable to the effect of cold therapy that led to a temporary reduction of spasticity for about 60–90 min. This enabled the therapist to promote normal patterns of hand function and attempt to “break” the learned abnormal motor patterns through continuous training of fine motor skills. Moreover, improvement of fine skills was attributable to higher improvement in wrist and elbow extension. This explanation is in agreement with O’Driscoll et al. [40] who said that achieving the majority of manipulative skills and good grip strength needs wrist extension.
Also, this study supports the work of Semenova et al. [41]who studied interference and needle EMGs of the forearm muscles after local cryotherapy application onto hands. They found that the cryotherapy produced a reduction of spasticity and increased the functional possibilities of the hand so that the writing became possible.
Conclusion
The results of this study provide evidence that the combination of cold therapy and conventional physical and occupational therapy experienced by children with spastic cerebral palsy can reduce spasticity and can translate into practical functional gains in the hand function. Cooling was used to reduce spasticity, enabling physical and occupational therapy training to be initiated for appropriate motor skills learning without the interfering spasticity. Finally, cold therapy is essential in preparing children with spastic cerebral palsy for subsequent physical and occupational therapy, which should be given immediately following cold therapy application. Further studies are needed to evaluate the effect of cold therapy in combination with splints, and also with neuromuscular electrical stimulation on hand function in children with spastic cerebral palsy. Also, studying the effect of cold therapy on speed of movement and hand function in children with dyskinesia is needed.
Acknowledgements
The authors would like to express their appreciation to all the children and their parents for their co-operation and participation in this study.